 |
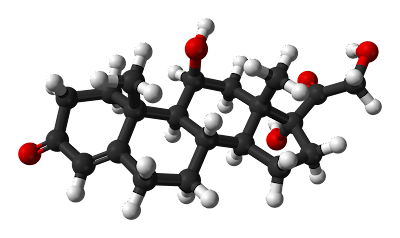
| The cortisol molecule. Don't you love these stick-and-ball molecular models? I do. I'd also like to see one for a McDonalds' Chicken McNugget. |
The hypothalamic-pituitary-adrenal axis (HPA or HTPA axis), also known as the limbic-hypothalamic-pituitary-adrenal axis (LHPA axis) and, occasionally, as the hypothalamic-pituitary-adrenal-gonadotropic axis, is a complex set of direct influences and feedback interactions among the hypothalamus, the pituitary gland (a pea-shaped structure located below the hypothalamus), and the adrenal (also called "suprarenal") glands (small, conical organs on top of the kidneys).
The interactions among these organs constitute the HPA axis, a major part of the neuroendocrine system that controls reactions to stress and regulates many body processes, including digestion, the immune system, mood and emotions, sexuality, and energy storage and expenditure. It is the common mechanism for interactions among glands, hormones, and parts of the midbrain that mediate the general adaptation syndrome.
The key elements of the HPA axis are:
The paraventricular nucleus of the hypothalamus, which contains neuroendocrine neurons that synthesize and secrete vasopressin and corticotropin-releasing hormone (CRH). These two peptides regulate:
The anterior lobe of the pituitary gland. In particular, CRH and vasopressin stimulate the secretion of adrenocorticotropic hormone (ACTH), once known as corticotropin. ACTH in turn acts on:
The adrenal cortices, which produce glucocorticoid hormones (mainly cortisol) in response to stimulation by ACTH. Glucocorticoids in turn act back on the hypothalamus and pituitary (to suppress CRH and ACTH production) in a negative feedback cycle.
CRH and vasopressin are released from neurosecretory nerve terminals at the median eminence. CRH is transported to the anterior pituitary through the portal blood vessel system of the hypophyseal stalk and vasopressin is transported by axonal transport to the posterior pituitary.
There, CRH and vasopressin act synergistically to stimulate the secretion of stored ACTH from corticotrope cells. ACTH is transported by the blood to the adrenal cortex of the adrenal gland, where it rapidly stimulates biosynthesis of corticosteroids such as cortisol from cholesterol.
Cortisol is a major stress hormone and has effects on many tissues in the body, including on the brain. In the brain, cortisol acts at two types of receptor -- mineralocorticoid receptors and glucocorticoid receptors, and these are expressed by many different types of neurons. One important target of glucocorticoids is the hypothalamus, which is a major controlling center of the HPA axis.
Vasopressin can be thought of as "water conservation hormone" and is also known as "antidiuretic hormone." It is released when the body is dehydrated and has potent water-conserving effects on the kidney. It is also a potent vasoconstrictor.
 |
| Book, books, and more books. I approve! |
Important to the function of the HPA axis are some of the feedback loops:
Cortisol produced in the adrenal cortex will negatively feedback to inhibit both the hypothalamus and the pituitary gland. This reduces the secretion of CRH and vasopressin, and also directly reduces the cleavage of proopiomelanocortin (POMC) into ACTH and β-endorphins.
Epinephrine and norepinephrine are produced by the adrenal medulla through sympathetic stimulation and the local effects of cortisol (upregulation enzymes to make E/NE). E/NE will positively feedback to the pituitary and increase the breakdown of POMCs into ACTH and β-endorphins.
Function:
Release of CRH from the hypothalamus is influenced by stress,physical activity, illness, by blood levels of cortisol and by the sleep/wake cycle (circadian rhythm). In healthy individuals, cortisol rises rapidly after wakening, reaching a peak within 30–45 minutes. It then gradually falls over the day, rising again in late afternoon. Cortisol levels then fall in late evening, reaching a trough during the middle of the night. An abnormally flattened circadian cortisol cycle has been linked with chronic fatigue syndrome, insomnia, and burnout.
Anatomical connections between brain areas such as the amygdala, hippocampus, and hypothalamus facilitate activation of the HPA axis. Sensory information arriving at the lateral aspect of the amygdala is processed and conveyed to the central nucleus, which projects to several parts of the brain involved in responses to fear. At the hypothalamus, fear-signaling impulses activate both the sympathetic nervous system and the modulating systems of the HPA axis.
Increased production of cortisol mediates alarm reactions to stress, facilitating an adaptive phase of a general adaptation syndrome in which alarm reactions including the immune response are suppressed, allowing the body to attempt countermeasures.
Glucocorticoids have many important functions, including modulation of stress reactions, but in excess they can be damaging. Atrophy of the hippocampus in humans and animals exposed to severe stress is believed to be caused by prolonged exposure to high concentrations of glucocorticoids. Deficiencies of the hippocampus may reduce the memory resources available to help a body formulate appropriate reactions to stress.
[
Stress and disease:
The HPA axis is involved in the neurobiology of mood disorders and functional illnesses, including anxiety disorder, bipolar disorder, insomnia, post-traumatic stress disorder, borderline personality disorder, ADHD, major depressive disorder, burnout, chronic fatigue syndrome, fibromyalgia, irritable bowel syndrome, and alcoholism.[
Antidepressants, which are routinely prescribed for many of these illnesses, serve to regulate HPA axis function.
Experimental studies have investigated many different types of stress, and their effects on the HPA axis in many different circumstances. Stressors can be of many different type -- in experimental studies in rats, a distinction is often made between "social stress" and "physical stress", but both types activate the HPA axis, though via different pathways. Several monoamine neurotransmitters are important in regulating the HPA axis, especially dopamine, serotonin and norepinephrine (noradrenaline). There is evidence that an increase in oxytocin, resulting for instance from positive social interactions, acts to suppress the HPA axis and thereby counteracts stress, promoting positive health effects such as wound healing.
The HPA axis is a feature of mammals as well as other vertebrates. For example, biologists studying stress in fish showed that social subordination leads to chronic stress, related to reduced aggressive interactions, to lack of control and to the constant threat imposed by dominant fish. Serotonin (5HT) appeared to be the active neurotransmitter involved in mediating stress responses, and increases in serotonin are related to increased plasma α-MSH levels, which causes skin darkening (a social signal in salmonoid fish), activation of the HPA axis, and inhibition of aggression. Inclusion of the amino acid L-tryptophan, a precursor of 5HT, in the feed of rainbow trout made the trout less aggressive and less responsive to stress.However, the study mentions that plasma cortisol was not affected by dietary L-tryptophan.
Studies on people show that the HPA axis is activated in different ways during chronic stress depending on the type of stressor, the person's response to the stressor and other factors. Stressors that threaten physical integrity, are uncontrollable or involve trauma tend to have a high, flat diurnal profile of cortisol release with lower than normal levels of cortisol in the morning and higher than normal levels in the evening, resulting in a high overall level of cortisol release during the day. Controllable stressors on the other hand tend to produce higher than normal morning cortisol. Stress hormone release tends to gradually reduce as time passes since the stress occurred. In post-traumatic stress disorder there appears to be lower than normal cortisol, and it is thought that a blunted hormonal response to stress may predispose a person to develop PTSD.
 |
| Here's the cortisol feedback loop at work. Cool, right? It seems many of the health concerns of today are made worse by modern stress, diet, and lifestyle on our still Flintstones-like bodies. |
Cortisol, also known more formally as hydrocortisone (INN, USAN, BAN), is a steroid hormone, more specifically a glucocorticoid, produced by the zona fasciculata of the adrenal gland. It is released in response to stress and a low level of blood glucocorticoids. Its primary functions are to increase blood sugar through gluconeogenesis; suppress the immune system; and aid in fat, protein and carbohydrate metabolism. It also decreases bone formation. Various synthetic forms of cortisol are used to treat a variety of diseases.


No comments:
Post a Comment